Many women experience pregnancy-related low back pain and/or pelvic pain. Pelvic Girdle Pain (PGP), also referred to as Pelvic Instability, is pain at the back of the pelvis, and/or pain over the pubic joint. It is important for pregnant women to understand this condition, and be aware of the treatment options, particularly if the pain is severe enough to interfere with their daily activities such as sitting, carrying and walking.
What is PGP?
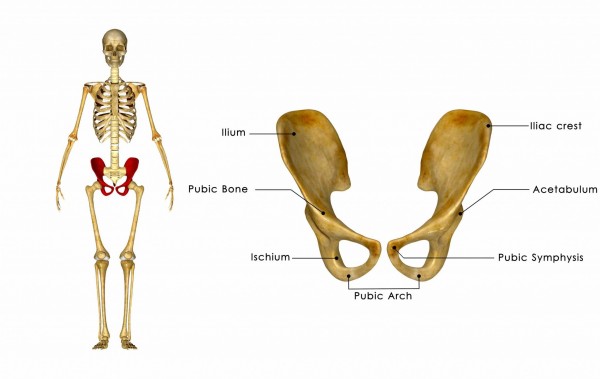
PGP is inflammation of one or more of the pelvic joints. There are two joints at the back of the pelvis (sacroiliac joints) and one at the front (pubic symphysis). Sacroiliac joint (SIJ) pain is generally located between the top of the pelvis and the buttock creases. Pubic symphysis pain is usually located over the pubic bone, groin, inner thigh and/or vaginal area.
What causes PGP?
PGP is very common and as many as 30% of all pregnant women experience PGP, which usually starts in the second trimester. The combination of pregnancy hormones, and rapid changes in posture and body weight both contribute to PGP. Genetics and lifestyle factors such as occupation and exercise may play a role too.
Reduced pelvic stability during pregnancy
The pelvic joints are extremely stable before pregnancy and only move by about 2 degrees. During pregnancy your pelvic joints become more mobile and moves up to 4 degrees. The feeling of ‘instability’ during pregnancy comes from suboptimal muscle control or dysfunctional movement patterns.
How do I know if I could have PGP?
You may have pregnancy-related PGP if you experience pain during daily activities listed below:
- Pain in one or both sides of the lower back/pelvic area
- Pain over the pubic bone
- Pain with rolling in bed
- Pain with standing up from a chair
- Pain whilst standing on one leg
If you suspect that you may have PGP see your physiotherapist, who will test the stability, movement and pain of your pelvic joints and muscles.
How do I treat it?
RICE management: The use of the following acronym is a helpful tip to remember what may help to decrease your pain.
- Rest – horizontal rest is the only way to offload the sore joints
- Ice – ice is a natural anti-inflammatory, and has a cumulative effect, so use it a lot!
- Compression – support garments such as tubigrip, a pelvic support belt or pregnancy shorts may help. Beware, in some cases these garments may make it worse. Seek advice from your women’s health physiotherapist first.
- Education – Talk to your physiotherapist for advice on changing your daily activities, exercise and posture to help decrease your pain. For more information, Fitwise Physiotherapy have an e-book on: PGP during pregnancy and as a New Mum: Management and Solutions
Additional techniques that may help:
- Manual therapy from your physiotherapist
- Decrease the amount of walking you are doing
- Avoid standing on one leg i.e. sit down to get dressed, avoid pushing things out of the way with your foot
- Clinical pilates to address your biomechanics
Can I still exercise?
YES! Exercise during pregnancy is good for you and your baby. Keep it low impact and pelvis friendly and your options could include:
- Pilates
- Stationary cycling
- Swimming (avoid breast stroke kick)
- Light weights sitting on a fitball or with weight even through both feet (avoid lunges or single leg movements)

Will it go away after I give birth?
Usually the pain improves when the cause (pregnancy) has been taken away. However, the higher the pain during pregnancy, the more likely the woman will have pain after pregnancy. Therefore, it is best to see a physiotherapist as soon as you can to help keep the pain at a low level during pregnancy. Research shows that functional rehabilitation (Pilates) after birth improves your post-natal outcomes, and decreases the change of PGP with subsequent pregnancies.
Credit image: onedollarphoto.com
Article from: www.fertilitypharmacy.com.au
