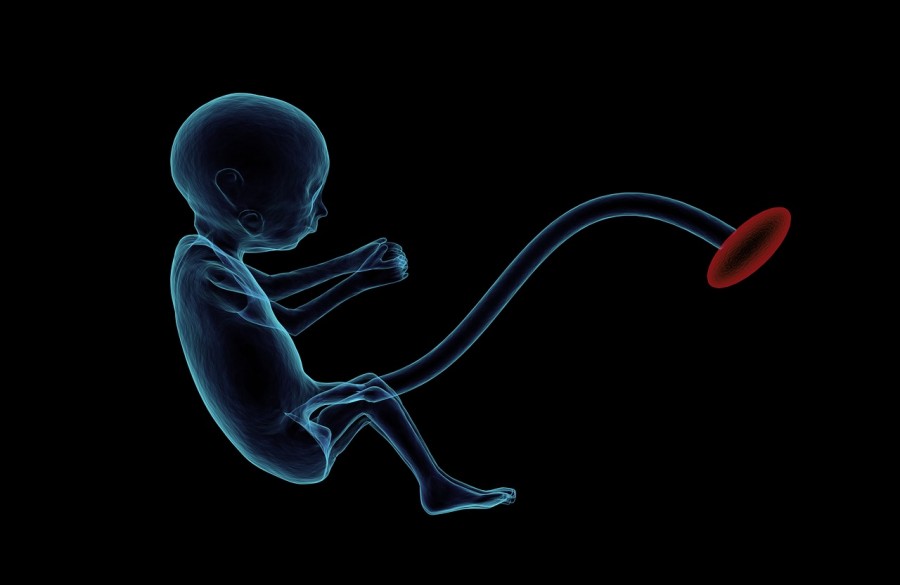
Antenatal tests are an important part of ensuring a healthy pregnancy. They can help you and your health professionals find out whether you are at risk of having a baby with chromosomal abnormalities or other congenital conditions.
Chromosomal abnormalities are when there are missing or extra genetic materials, which can lead to physical and/or intellectual disability. Some chromosomal abnormalities include the Down syndrome, Edwards syndrome and Patau syndrome.
There are other congenital defects that may develop in pregnancy, which are not caused by chromosomal abnormalities. These include neural tube defects such as spina bifida.
Screening tests vs diagnostic tests
Screening tests are tests that assess the risk of your baby having certain known chromosomal abnormalities or conditions. They are not the ultimate tests for diagnosing a condition, so won’t tell you if your baby is definitely affected. Screening tests also don’t detect all possible chromosomal abnormalities, but the more common ones.
To be certain whether your baby has a condition or not, diagnostics tests are required after the screening tests return concerning results. These tests can pick up a wider range of abnormalities and can usually give you a yes or no answer to a certain condition.
It is perfectly understandable that being given high-risk results from a screening test is nerve-wracking. If it does happen, be sure to discuss thoroughly with your health professional what this could mean. Would you and your partner like to go on to take a diagnostic test or are you comfortable dealing with a familiar medical condition after birth even without a definitive test result?
Non-invasive prenatal testing (NIPT)
NIPT is a simple blood test that can be done any time from 10 weeks of pregnancy onwards to determine your baby’s risk for certain genetic abnormalities. It uses small fragments of DNA that are free-floating in the mother’s bloodstream, which contains some DNA from the placenta. Since the placental DNA is usually identical to the DNA of the baby, it provides a safe opportunity for early detection of genetic abnormalities. As such, NIPT may also be called cell-free DNA or cfDNA testing.
Conditions that NIPT can screen for include:
- Down syndrome
- Trisomy 18
- Trisomy 13
- Missing/extra sex chromosomes
Combined first trimester screening (CFTS)
When a pregnant woman receives a low risk NIPT result, it provides high confidence that the pregnancy is not affected by some of the most common chromosomal abnormalities. However, CFTS may still provide useful information relevant to the management of the pregnancy. For example, it is estimated that 17% of women who got increased risk on their CFTS result returned an abnormal chromosome result that would otherwise be undetected by NIPT.
CFTS combines a blood test with a 12-week ultrasound scan. The blood tests can be done at 8-12 weeks of pregnancy and involves measuring the levels of two hormones. Abnormal levels of these biochemical signals could indicate risk of chromosome abnormality not detected by NIPT.
With the ultrasound, the professional will measure the amount of fluid in the skin at the back of the baby’s neck, which is called the nuchal translucency (NT). All babies will have some fluid at the back of their neck, but when there is more fluid than usual, the babies may be suspected for Down syndrome or Edward syndrome. The absence of nasal bone could also be an indicator of increased risk of Down syndrome.
Even with a low risk NIPT result, increased NT is associated with miscarriage, intrauterine death and other structural defects and genetic syndromes. More testing may be suggested by your health professional in this case.
Second trimester maternal serum screening
This screening also looks at the risk of certain chromosomal abnormalities, but by using different markers. The test itself involves a simple blood test between 14 and 20 weeks of gestation. It measures hormones from your placenta and your baby. The levels of these hormones, your and your baby’s age are combined to give a final chance of Down syndrome, Edward syndrome and neural tube defects. The result could be a low chance result or an increased chance.
Note that a low chance does not necessarily rule out a genetic condition and an increased chance does not say for sure that a baby has a condition. In fact, most women with an increased chance result will not have a baby with the mentioned defects. Nevertheless, these women should be offered further diagnostic testing such as the chorionic villus sample (CVS) and amniocentesis.
Chorionic villus sampling
CVS is a more invasive test compared to the previous screening tests as it needs a sample from the placenta. This involves a local anaesthetic for your tummy area, followed by guiding a thin needle using ultrasound in your uterus.
CVS is best done in the first trimester, between 10 and 13 weeks. The results generally take up to two weeks, which can be painful to wait for. CVS also comes with some risks because 1 out of 500 times when a CVS is done, there will be a miscarriage that would not have happened otherwise.
Amniocentesis
Amniocentesis is an alternative to the CVS test. Sometimes, you may be offered the test when the CVS results alone are not clear enough. Amniocentesis is used further along the pregnancy in the second trimester between 15 and 20 weeks of pregnancy, and the results could take up to a few weeks.
Amniocentesis requires a sample from the amniotic fluid surrounding your baby. The collection process is similar to that for CVS, meaning that it comes with similar risks, including:
- Leaking of amniotic fluid
- Slight risk of miscarriage
- Needle injury
- Rh sensitisation
- Infection
Generally, CVS or amniocentesis are only suggested to reveal whether a baby has the suspected birth defects. For example, if the results of a screening test is worrisome, or if you have a specific genetic condition in the family history. Ultimately, the decision to have these diagnostic testing or not are up to you, and your health care provider or genetic counsellor can help with your decision-making process.
If you are still unsure about having or interpreting an antenatal test, you could contact Melbourne-based obstetrician, Dr. Alex Polyakov here.