Largely due to today’s career and culture shift, women worldwide are giving birth later in life. For example, the average age of births was 25.4 years following the second World War, but it rose sharply to 30.6 years in 2017. Thanks to advancing fertility preservation technologies, many modern women have the option to “stop” their biological clock by freezing their eggs.
Apart from optional fertility preservation for social reasons, there are also patients who desperately need the technology. For example, cancer is a major health concern and usually involves harsh treatment that is commonly detrimental to reproductive function. Unfortunately, young cancer survivors are at a high risk of losing their fertility after chemotherapies. While they can recover from cancer, the loss of fertility is often permanent as women are born with all the eggs that they will ever have.
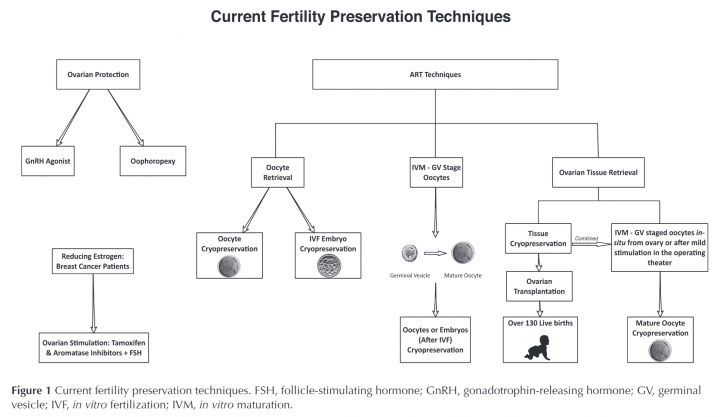
To prevent treatment induced fertility damage, women are now generally offered fertility preservation options before undergoing cancer therapies.
Mature egg cryopreservation (freezing)
The most widely used fertility preservation technique is egg freezing, which starts by stimulating the production of multiple eggs using hormones. Ovarian stimulation lasts for 10-12 days, enabling usually 6-15 eggs to mature. The eggs are then collected from the ovaries using an ultrasound guided probe and taken to the laboratory. From there, the eggs undergo a freezing procedure called vitrification, allowing the eggs to be stored for many years.
This method might remind you of the process of IVF, and they are indeed similar. IVF cycles usually start with the same ovarian stimulation, egg pickup and freezing. Frozen eggs can be thawed at a later date, fertilised, and transferred back to a woman’s uterus in what’s known as the “frozen embryo transfer”.
In one study of 176 cancer patients who underwent egg cryopreservation by either slow freezing or vitrification, 10 patients returned for fertility restoration. The live birth rate was 44% per embryo transfer cycle, similar to patients without cancer.
Although egg freezing is routinely performed in fertility clinics with great success, it may not be a viable choice for women requiring urgent cancer treatment as the ovarian stimulation protocol takes days. Also, certain types of cancer are hormone-sensitive, meaning that ovarian stimulation could potentially further complicate the patient’s cancer condition.
Ovarian tissue cryopreservation
Ovarian tissue cryopreservation is an alternative preservation technique that does not require ovarian stimulation. Instead of individual egg, some ovarian tissue is harvested during a surgical procedure and frozen before cancer treatment commences. When the patients wish to get pregnant, the ovarian tissue can be transplanted back in a second surgery.
The first live births from implanted frozen-thawed ovarian tissue were reported in Belgium and Israel. To date, more than 130 live births have been documented worldwide.
This technique is suitable for prepubertal girls and patients requiring urgent treatment; however, it does require two surgeries and carries the risk of reintroducing malignant cells at transplantation. For example, transplanting ovarian tissue back in blood cancer survivors can be riskier. The success rate of tissue grafting is variable as it also depends on the surgeon’s experience.
In vitro maturation
In vitro maturation (IVM) is a new fertility preservation method that was first applied in patients with polycystic ovaries syndrome (PCOS), who are at high risk of developing ovarian hyperstimulation syndrome (OHSS) after hormonal stimulation.
IVM involves the retrieval of immature eggs from ovaries after minimal or no hormonal stimulation and then either immediate cryopreservation or at matured stage after IVM. Since immature eggs are not competent yet in being fertilised, they need to be grown in specialised culture medium that attempts to mimic a woman’s ovary.
To date, the clinical outcome of IVM is still suboptimal as lab matured eggs are likely not as good as those matured in a woman’s ovary. As such, IVM procedure is considered as experimental and researchers worldwide are working on optimising the in vitro culture conditions.
Having said that, IVM does bring some notable advantages. It eliminates the risk of reseeding cancer and allows for fertility preservation without hormonal stimulation or delays in cancer treatment. By removing the need to administer hormones, IVM avoids costly drugs and frequent monitoring.
In Australia, immature oocytes were first collected from patients with PCOS, resulting in one live birth in 1994. The first live births using frozen-thawed embryos from in vitro-matured oocytes of cancer survivors were reported in Singapore, Belgium, and the United States.
Ovarian protection medications
Currently, the only medication for ovarian protection during chemotherapy is gonadotrophinreleasing hormone (GnRH) agonist. However, its efficiency remains controversial.
In 2013, The American Society for Reproductive Medicine recommended the use of GnRH agonist in combination with other fertility preservation methods, such as one discussed above.
For more information regarding fertility preservation, you can contact Melbourne-based fertility specialist and gynaecologist, Dr Alex Polyakov here.
