Many countries are ramping up measures to flatten the curve for the COVID-19 pandemic, especially the UK, which previously showed signs of letting herd immunity take its course. Massive policy changes were partly due to a recent epidemiological modelling report on non-pharmaceutical interventions by the Imperial College of London, which concluded: epidemic suppression is the only viable strategy at the current time.
The study considered the impact of five different non-pharmaceutical interventions:
- Symptomatic case isolation at home for 7 days
- Voluntary home quarantine for 14 days
- Social distancing of those over 70 years old
- Social distancing of entire population
- Closure of all schools and 75% of universities
Without any control measures, mortality rate is expected to peak in three months and 81% of the UK and US populations would be infected. As a result, critical care bed capacity would be far exceeded way before reaching the peak. If the virus is let to run its course, the critical care bed demand would be 30 times more than the maximum capacity at the predicted peak. As more stringent control measures are put into the equation, the curve starts to flatten.
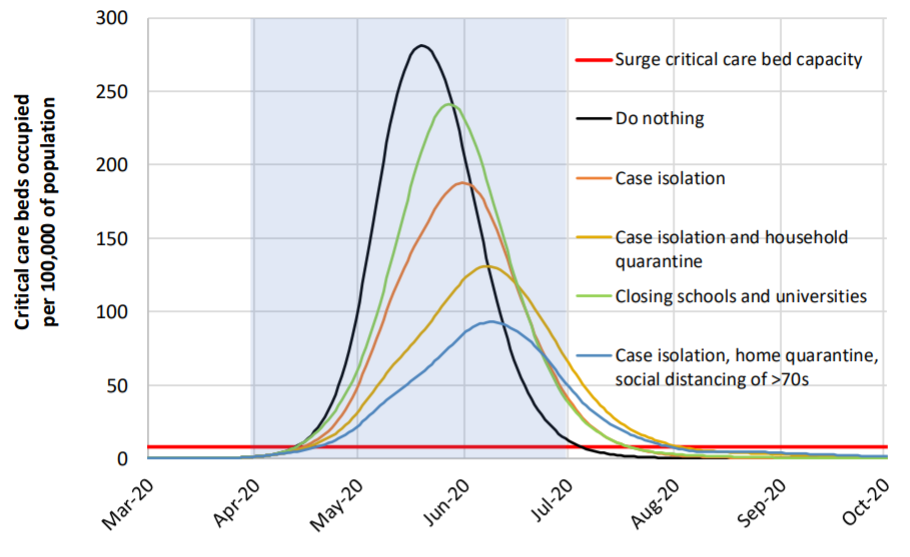
The study next modelled the relative impact by each intervention strategy on the deaths and ICU capacity. The most effective combination of actions is the strictest one: case isolation + social distancing of the entire population + home quarantine + school and university closure, assumed to stay in place for 5 months. Among them, case isolation and household quarantine are core epidemiological interventions that reduce onward transmission.
If these measures can be implemented, COVID-19’s reproduction number, R, may be reduced to under 1. This is a key indicator for a successful suppression strategy, in which case numbers are low enough to eliminate human-to-human transmission.
By contrast, loose interventions that aim for mitigation only reduce the health impact of the epidemic, rather than stopping the transmission completely. With mitigation, the R will not be lowered to 1 from a current estimate of 2.4. Although a mitigation strategy can also reduce the death rate and burden on healthcare systems, the demand for critical care beds will still exceed the maximal capacity at least 8 times.
Therefore, the study concluded that epidemic suppression, rather than mitigation, is the only viable strategy for controlling COVID-19. In order to see rapid improvements on the situation and prevent a rebound in transmission, the suppression interventions need to start as early as possible and stay in place until mass production of vaccines is available to, which could take another 18 months.
